Physician Associate Question Bank and Virtual Textbook
PA Practice is an unrivalled resource for physician associate students studying in the UK. It provides over 3,000 questions in a fully customisable quiz experience, alongside disease summaries which outline high yield examinable material on over 350 conditions to form a complete learning platform.
PA Practice has an ever-evolving question bank, with over 3,000 bespoke multiple choice questions on over 350 conditions from the physician associate clinical matrix

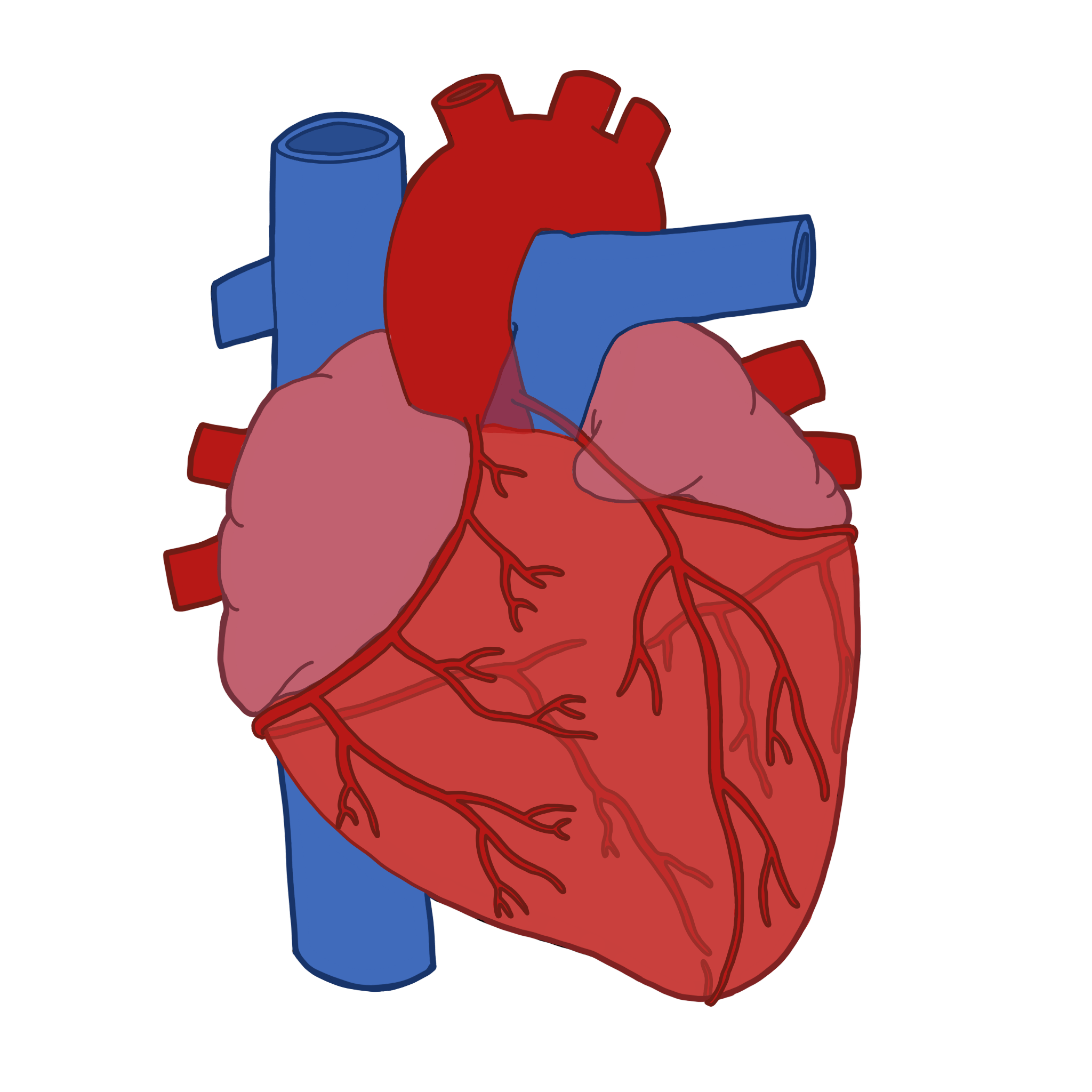
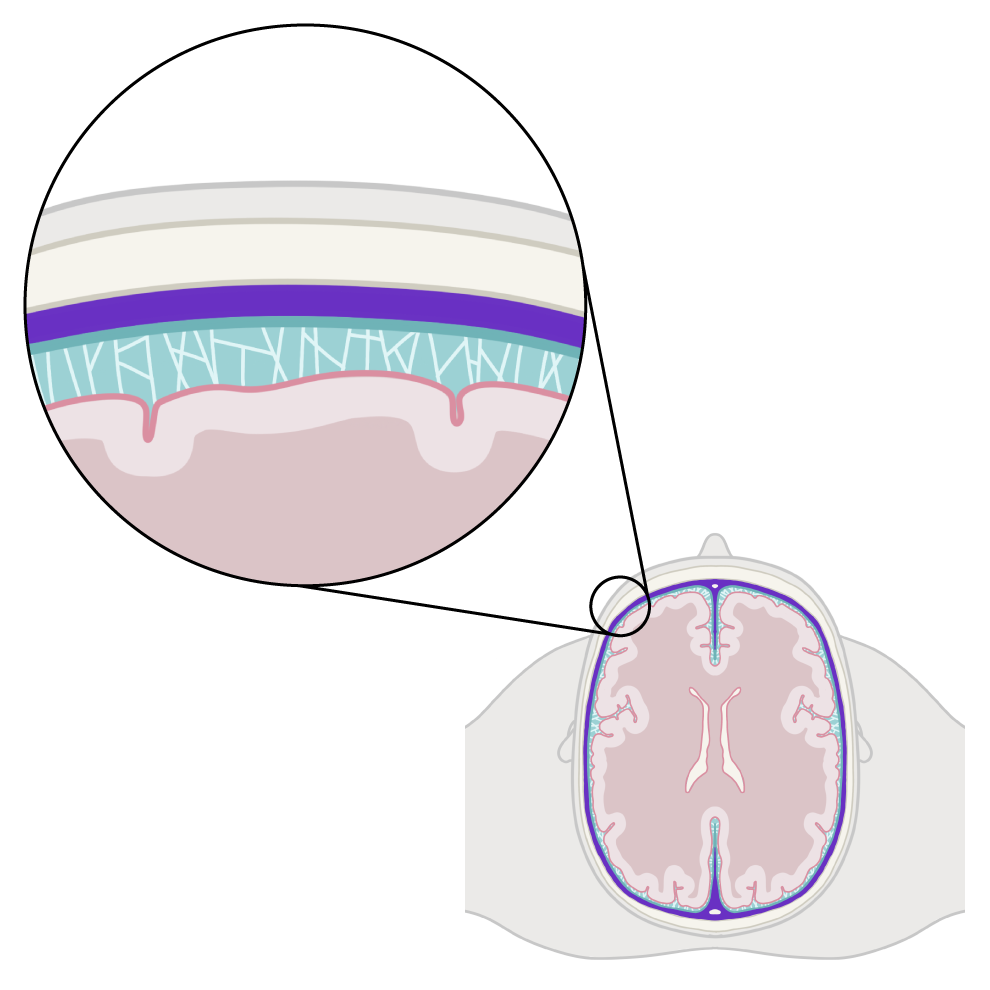
Professional medical illustrations have been created in collaboration with a qualified PA to illustrate complex medical concepts in an easy-to-understand manner
There is high yield information on over 350 conditions from the matrix, which summarises relevant definitions, anatomy and physiology, pathophysiology, symptoms, signs, investigations, and management for each disease
see example below
Definition
Acute pericarditis involves acute inflammation of the pericardium.
Etymology
Peri (“around”) card (“of the heart”) itis (“inflammation”). Pericarditis literally means inflammation of that which surrounds the heart.
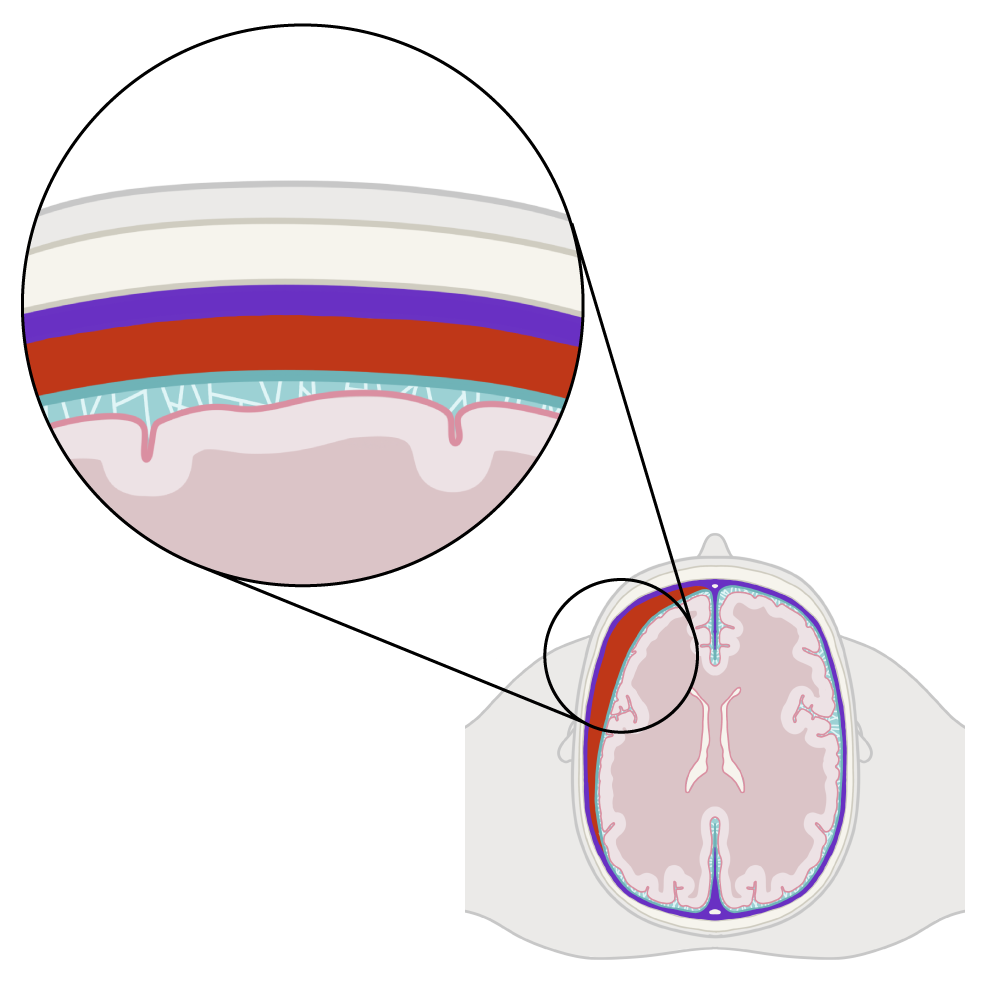
Anatomy and Physiology- The Pericardium
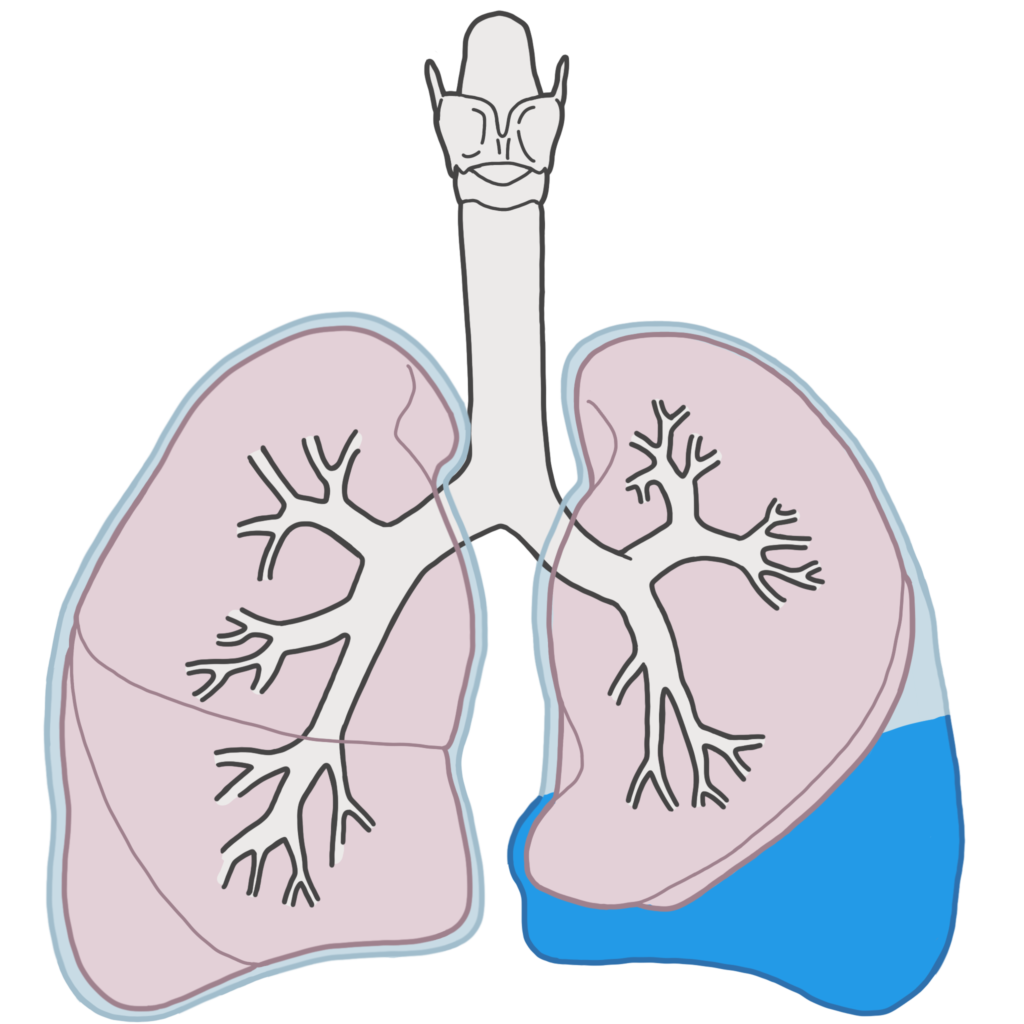
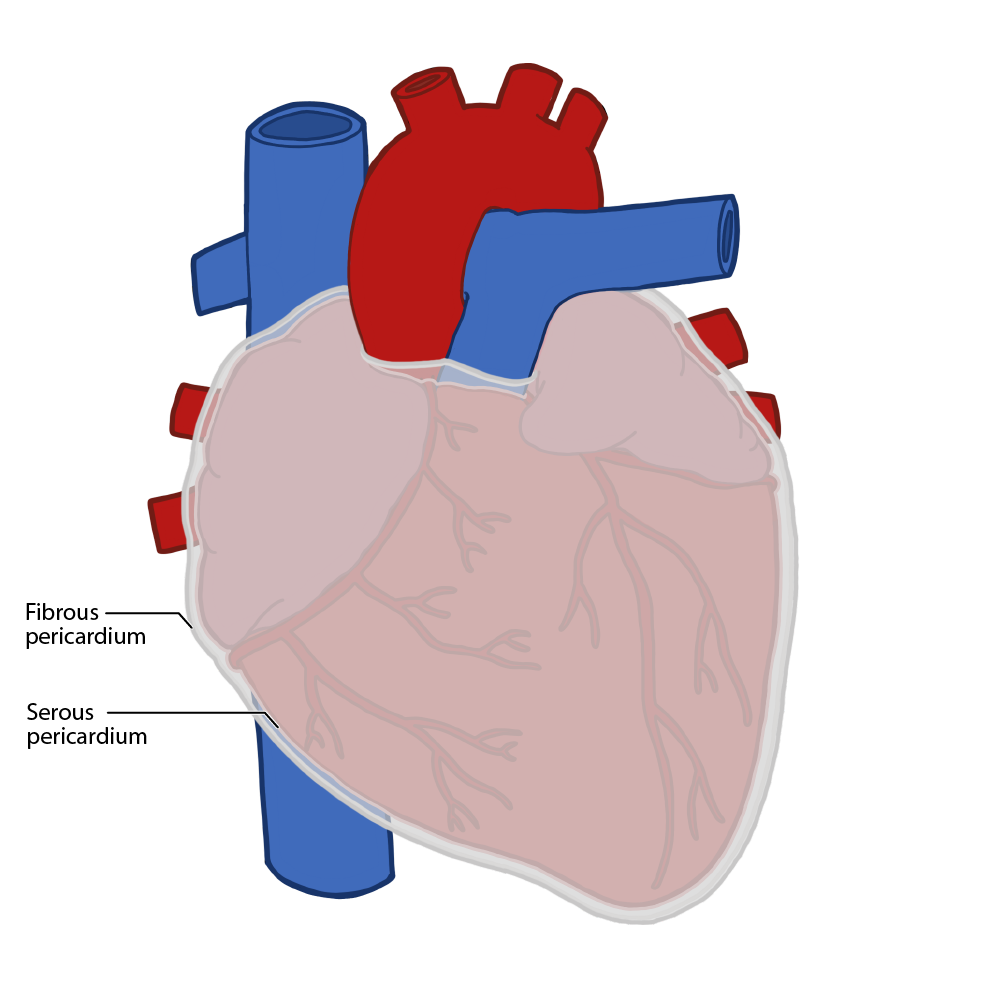
The heart is located within a fluid filled sack called the pericardium. The pericardium has two layers; the fibrous and serous pericardium. The outer fibrous pericardium forms a thick outer shell that surrounds and protects the heart. The inner serous pericardium is split into two layers. One layer lines the inner surface of the fibrous pericardium, while the other lines the outer surface of the heart. The layer which surrounds the heart is also known as the epicardium. There is a small amount of fluid present within the space between the two layers of serous pericardium. Serous fluid is produced by cells within the serous pericardium to lubricate the interface between the two layers of pericardium and ensure there is no friction between the heart and the pericardium as the heart contracts and relaxes.
Pathophysiology
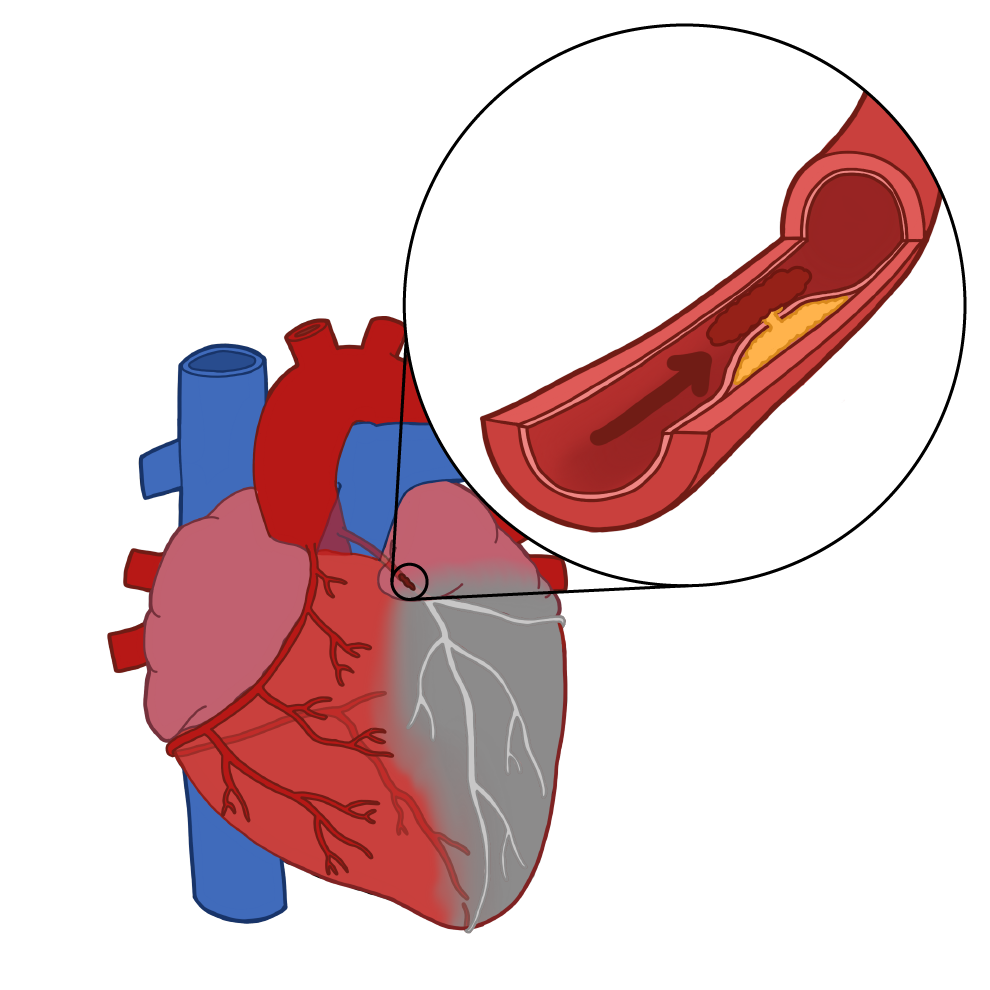
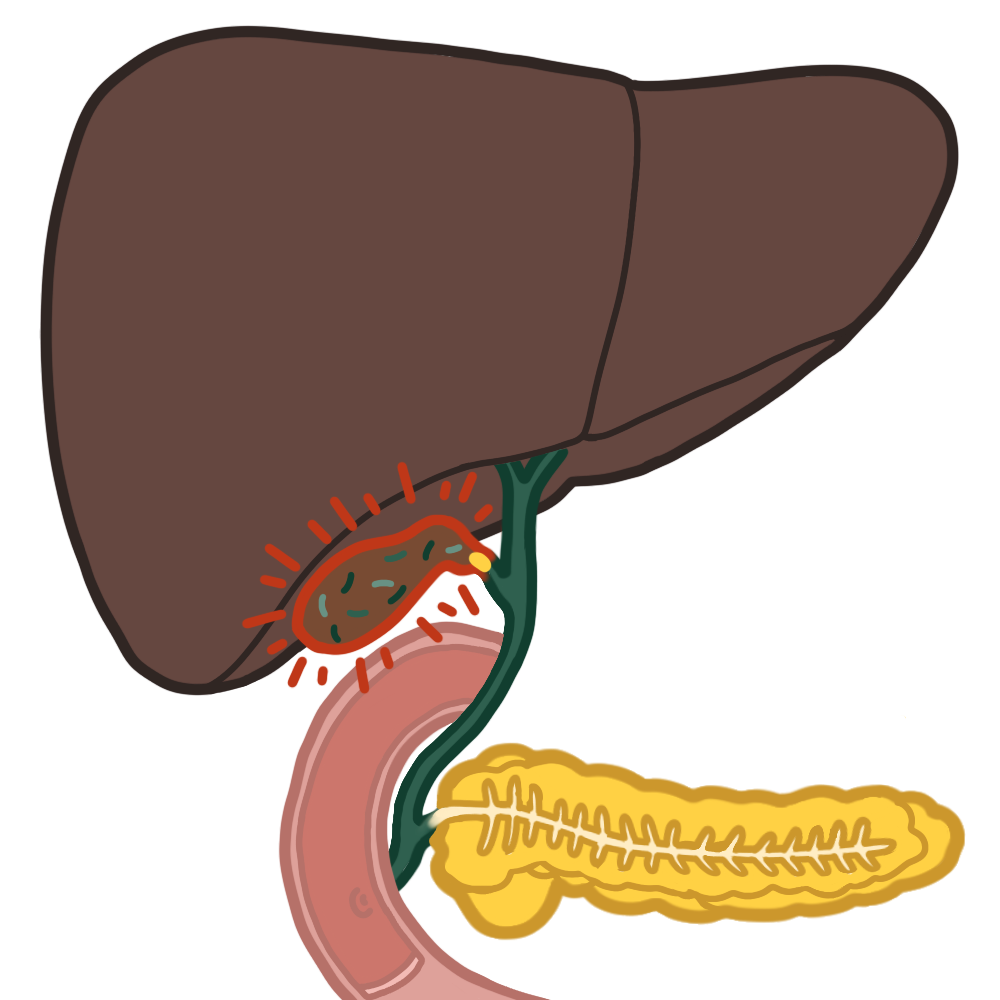
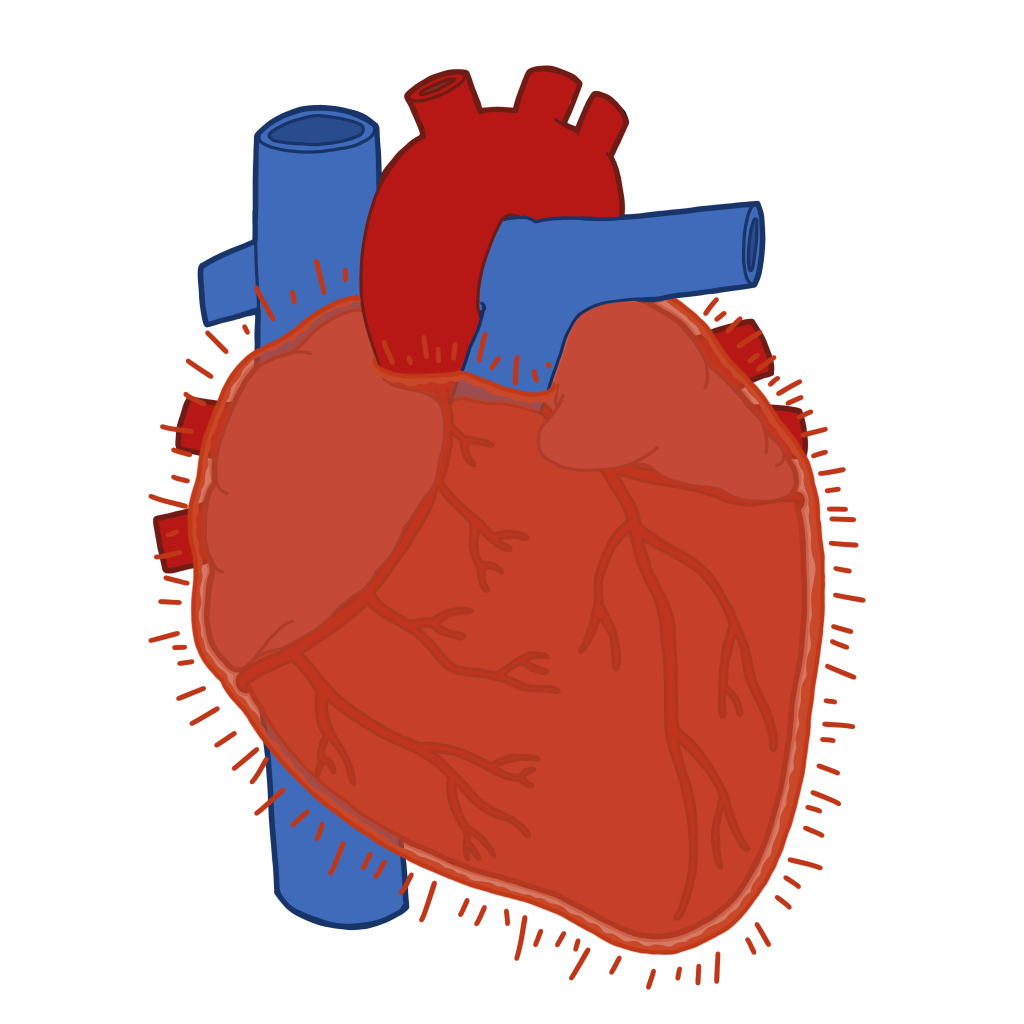
Acute pericarditis involves acute inflammation of the pericardium. There are several causes of pericarditis, including viral infection, myocardial infarction, metastatic disease, autoimmune disease, and trauma. Viral infection is the most common cause. Sars-cov-2 and coxsackie B are common causative viruses. No matter the cause, inflammation of the pericardial tissue results in a multitude of symptoms. The fibrous pericardium is a direct continuation of the diaphragm, and as such is also innervated by the phrenic nerve. Those with pericardial pathology, like pericarditis, subsequently experience referred pain to the shoulder as a result of activation of the phrenic nerve and it’s associated nerve roots (C3-5). Inflammation irritates the nerve fibres of the phrenic nerve, leading to a characteristic type of chest pain. Patients often experience a sharp, stabbing central chest pain. The pain is pleuritic, as when the diaphragm moves during breathing, the pericardium is irritated further. The pain may radiate to the shoulder or neck due to irritation of the phrenic nerve and stimulation of the C3-5 nerve roots. The pain is commonly much worse when lying flat, as the abdominal contents are displaced superiorly when lying supine, irritating the pericardium. Conversely, the chest pain of pericarditis is relieved when sitting up and leaning forward, as the heart and pericardium are no longer irritated by the abdominal contents when leaning forward. Inflammation reduces the efficacy of the lubricating functions of the pericardium. The heart and pericardium subsequently rub against one another, which can be heart upon auscultation as a pericardial friction rub. A friction rub sounds like two sheets of sandpaper rubbing against one another.
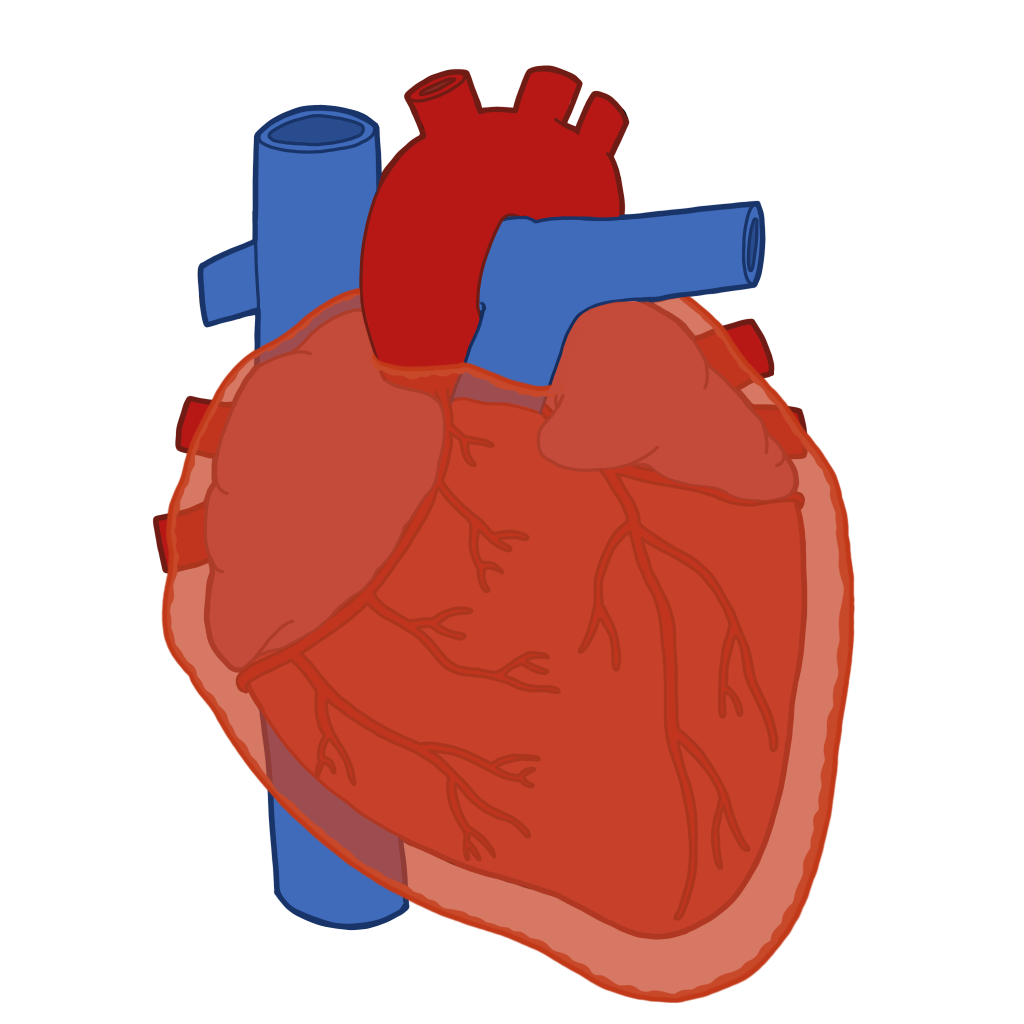
Inflammation of the fluid producing serous layer of the pericardium commonly leads to pericardial fluid overproduction. Inflammation involves the release of numerous inflammatory cytokines which promote vasodilation and increase vascular permeability. This can lead to abnormal fluid accumulation within the pericardial cavity. This process is termed pericardial effusion, and is a common complication of pericarditis. It is thought that over 50% of patients with pericarditis experience some degree of pericardial effusion. Pericardial effusions are often small, and do not go on to cause significant symptoms.
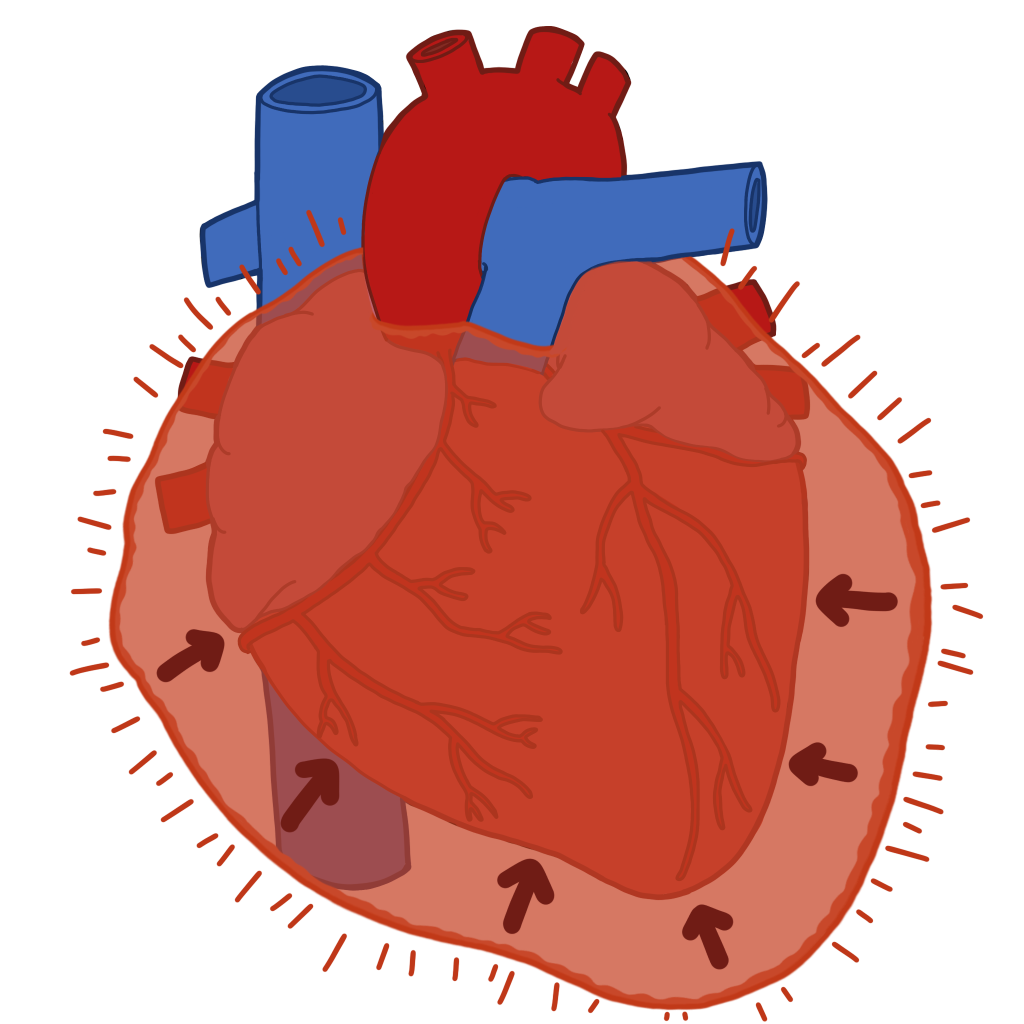
Large pericardial effusions can have rapidly fatal consequences. Fluid accumulation within the pericardial cavity can eventually lead to a build up of enough pressure to compress the heart and the great vessels. This process is termed cardiac tamponade. Cardiac tamponade leads to drastic reductions in venous return, ventricular filling, and ultimately cardiac output. It is extremely important to understand the signs and symptoms of cardiac tamponade, as it is a rapidly fatal but treatable condition. Build up of large amounts of fluid muffles the normal heart sounds, as the sound waves are absorbed by the excess pericardial fluid. Compression of the SVC and IVC leads to venous congestion, causing a raised JVP and peripheral oedema. Muffled heart sounds, a raised JVP, and hypotension form the triad of signs and symptoms associated with cardiac tamponade called Beck’s triad. Venous return increases during inspiration, which leads to an interesting and specific sign of tamponade. When venous return increases during inspiration, the right side of the heart takes up more of the confined space within the pericardial sac. This compresses the left side of the heart during inspiration, which causes a reduction in cardiac output and subsequently blood pressure during inspiration. This phenomenon is termed pulsus paradoxus, and is a relatively specific sign of cardiac tamponade. In those with large effusions, the whole heart moves within the fluid which can produce beat to beat alterations in the size of the QRS complexes as the heart moves further or closer to the electrical leads. This is termed electrical alternans, and is another relatively specific sign of cardiac tamponade.
- Pleuritic chest pain
- Pain relieved upon sitting forward
- Pain exacerbated when lying flat
- +/- pain radiation to the shoulder
- Pericardial friction rub
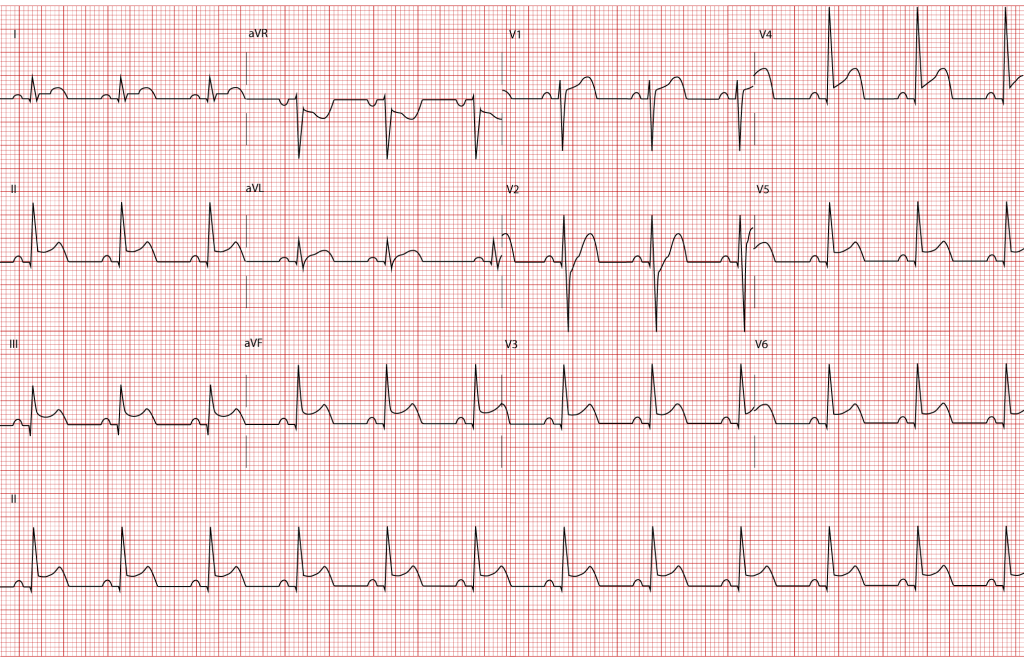
- ECG- ECG is diagnostic in those with pericarditis. The ECG findings in those with pericarditis are alarming, as patients stereotypically have diffuse ST elevation effecting multiple leads, as below. It is extremely important to rule out STEMI in those with widespread ST elevation. Understandably, this is difficult to distinguish from MI. The ST elevation of those with pericarditis is not confined to regional leads as in those with STEMI. The ST elevation in those with pericarditis is saddle shaped, or concave. PR depression is another common finding in those with pericarditis, but is not illustrated below. Pericarditis is not associated with new onset conduction disorders like AV block or LBBB, as in MI. The ECG should also be assessed for signs of large effusions or tamponade. As the electrical current has more dense medium to travel through in those with pericardial effusion, the QRS voltage is commonly reduced. As mentioned above, the QRS voltage may have beat to beat alterations, this is termed electrical alternans, and is secondary to movement of the heart within excess pericardial fluid in those with large effusions or cardiac tamponade.
- Echocardiography- Echocardiography is the gold standard to rule out pericardial effusion and cardiac tamponade. It accurately assesses the amount of fluid and its impact on cardiac function. Large effusions can cause collapse of the right side of the heart which may be visible if there is cardiac tamponade. Movement of the heart within the excess fluid can also be visualised. This is termed a “swinging heart”.
- Pericardiocentesis- A needle is inserted into the pericardial cavity to remove the excess fluid in those with large effusions. This has both diagnostic and therapeutic importance. The fluid can be sent for cytology to assess for risk of malignant causes if suspected, or sent for microbiological assessment if an infectious cause is suspected. Removal of the excess fluid also relieves the pressure within the pericardium, and is important in the management of large symptomatic pericardial effusions which are causing, or at risk of causing, cardiac tamponade.
- Routine bloods- FBC may reveal raised inflammatory markers in keeping with infection. U and Es should be assessed as uraemia can cause pericarditis.
- Troponin- It is important to assess cardiac markers as pericarditis can be caused by MI. Those with pericarditis commonly have widespread ST elevation upon ECG, and any patient with ST elevation of any kind should have troponin levels taken.
- Chest x-ray- CXR may reveal “water-bottle” sign in those with large pericardial effusions, as fluid accumulation makes the cardiac silhouette resemble a vase or “water-bottle”. CXR should also be carried out to rule out other important differentials in those presenting with chest pain
- NSAIDs- NSAIDs are used to manage pericarditis. NSAIDs act by inhibiting COX. COX is an enzyme which is involved in the formation of prostaglandins. Prostaglandins play a key role in both inflammation and pain sensation. NSAIDs help reduce pericardial inflammation and chest pain. Examples include high dose ibuprofen. PPI cover should be co-prescribed to protect against gastric ulceration.
- Colchicine– Colchicine is used to manage pericarditis. Colchicine can be used to further reduce inflammation if patients do not experience an improvement in symptoms after a course of NSAIDs. This can also be used long term to reduce rate of recurrence
- Steroids- Steroids can be used to manage pericarditis. Steroids are potent anti-inflammatory drugs. If pain and inflammation does not subside with NSAIDs, steroids may be required to inhibit inflammation. Their use is controversial, but generally accepted in specific cases, for example if the pericarditis is secondary to autoimmune disease like rheumatoid arthritis.
- Treat the underlying cause!- It is imperative that the underlying cause is identified and treated appropriately.
- Tamponade- Pericardiocentesis- Tamponade is an emergency which must be treated immediately. A needle is inserted into the pericardial sac to remove excess fluid in those who have developed symptomatic effusion or cardiac tamponade. Surgical intervention- If tamponade is not controlled with pericardiocentesis, or there is trauma or haemopericardium, surgical drainage may be required to control tamponade.
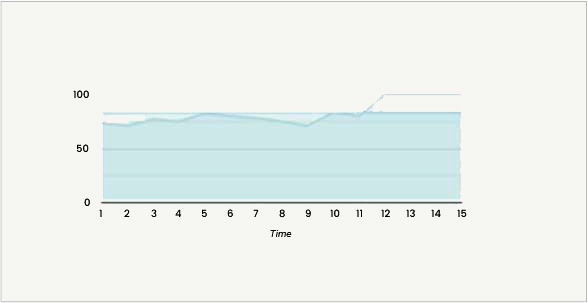
Sophisticated performance analytics have been designed to highlight areas of improvement and focus further study
Your Performance Over Time


Suggested Reading
Essential Hypertension
Average quiz performance: 30%
Bells's Palsy
Average quiz performance: 35%
Hypothyroidism
Average quiz performance: 40%
PA practice is a fully customisable quiz experience. Users can highlight specialties, or focus on specific diseases from the matrix
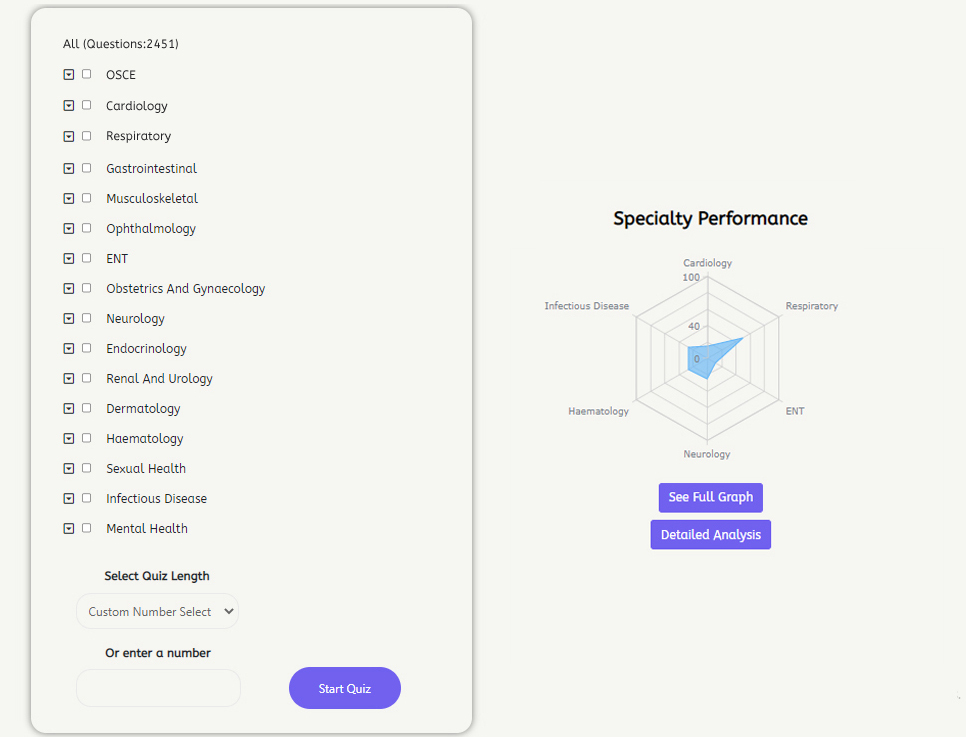
Practice for the national exam in the lead up to your physician associate national exam
Register now from less than £5 per month!
